Coronavirus (COVID-19) & Sickle Cell Disorder
Coronavirus (COVID-19) & Sickle Cell Disorder
This page provides the latest information and guidance specifically relating to coronavirus (COVID-19) and sickle cell. It also contains links to the general guidance and rules regarding coronavirus (COVID-19). [Updated 05/01/2022]
Contents
What is Coronavirus (COVID-19)?
COVID-19 is an illness that particularly affects the lungs and airways but can also affect the gut, kidneys, heart and brain . It is caused by a virus called coronavirus.
The main symptoms include high temperature and/or new and continuous cough. People with the infection often notice a loss of taste and smell. Symptoms may be mild during the first week and then worsen after about 10 days. As time goes on and more knowledge has been gained about the nature of the virus, it has become apparent that there can be long term effects of COVID-19 infection
As the illness is new, there is limited specific information for people living with sickle cell. However, below we have included all the available specific information there is and included the official guidance on avoiding catching or spreading germs and what to do if you need medical help, which all apply.
Staying alert and safe – for all
The official government guidance around Coronavirus (COVID-19) continues to be updated with new rules around national and local restrictions. You can be kept up-to-date with all the latest general information here: https://www.gov.uk/coronavirus
England is moving to Plan B in response to the risks of the Omicron variant.
- Wear a face covering in most indoor public places and on public transport
- Get tested and self-isolate if required
- Work from home, if you can
- Get vaccinated
- Let fresh air in if you meet indoors. Meeting outdoors is safer
You can find the specific rules about what you can and cannot do here: https://www.gov.uk/guidance/covid-19-coronavirus-restrictions-what-you-can-and-cannot-do
For clinically extremely vulnerable from COVID-19 (adults with sickle cell disorder)
For people who fall into the clinically extremely vulnerable category (adults with sickle cell disorder), you should first look at the general guidance found above and any specific guidance for your area.
Information on advice for the clinically extremely vulnerable group can be found here: www.gov.uk/government/publications/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19
Plans for Future Shielding
Given the improved protections against the virus (vaccines and treatments), and the known
harms to physical and mental wellbeing that shielding can cause, the current clinical advice is that it
is not appropriate to reintroduce shielding.
Those in the clinically extremely vulnerable group are advised to follow the national restrictions and guidance.
You can find more details about the national restrictions here: www.gov.uk/government/publications/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19
Some of this guidance is specific to England, you can find more specific guidance for Wales, Scotland and Northern Ireland here:
Wales: https://gov.wales/shielding-extremely-vulnerable-people
Scotland: www.gov.scot/publications/covid-shielding/
Northern Ireland: https://www.nidirect.gov.uk/articles/guidance-shielding-extremely-vulnerable-people
Vaccine
As you may be aware, vaccination for COVID-19 is widely available across the UK. We welcome the news that there is a vaccine available to help protect against COVID-19 infection. In partnership with the National Haemoglobinopathy Panel, the UK Forum on Haemoglobin Disorders and the UK Thalassaemia Society we have issued a statement along with information specific to the COVID-19 Vaccination in patients with Haemoglobinopathies and Rare Inherited Anaemias (including sickle cell disorder). Click here to read the full statement.
Third Dose and Booster Dose
The Joint Committee on Vaccination and Immunisation (JCVI) is advising that people with severely weakened immune systems should have a third vaccine dose as part of their primary COVID-19 vaccination schedule. Find out more by reading the full announcement here: https://phe-newsroom.prgloo.com/news/jcvi-issues-advice-on-third-dose-vaccination-for-severely-immunosuppressed
The third dose is offered to people over 12 who were severely immunosuppressed at the time of their first or second dose, including those with sickle cell.
This affects around half a million people and the NHS will contact you as soon as possible to discuss your needs and arrange an appointment for a third dose where clinically appropriate. Some individuals who are immunosuppressed due to underlying health conditions or medical treatment may not achieve the same full immune response to the initial 2 dose COVID-19 vaccination course as those who are not immunosuppressed.
In response to the emergence of Omicorn variant, the JCVI advises that severely immunosuppressed individuals who have completed their primary course (3 doses) should be offered a booster dose with a minimum of 3 months between the third primary and booster dose. Those who have not yet received their third dose may be given the third dose now to avoid further delay. A further booster dose can be given in 3 months, in line with the clinical advice on optimal timing.
How do people know if they’re eligible for a third dose?
This affects around half a million people and the NHS will contact you as soon as possible to discuss your needs and arrange an appointment for a third dose where clinically appropriate.
Will people who get the third dose still be eligible for a booster?
Yes. Severely immunosuppressed individuals will become eligible for a booster dose as part of a routine booster programme with a minimum of 3 months between the third primary and booster dose. Third doses are being given not to combat waning immunity but to bring these individuals up nearer to the same level of immunity as the non-immunosuppressed achieve from 2 doses.
Vaccines and Sickle Cell (Videos)
We are also working with various clinicians and patients to produce a three-part series of videos about sickle cell, COVID-19 and vaccinations. You can see the first two installments below:
Learn about the COVID-19 Vaccine with Dr Anna Goodman
Getting the COVID-19 Vaccine: Sickle Cell Patient Stories
Sickle Cell, COVID-19 & Vaccination (Presentation and Q&A)
COVID-19 Vaccines, Pregnancy and Breastfeeding
The COVID-19 vaccines available in the UK have been shown to be effective and to have a good safety profile. The early COVID-19 vaccines do not contain organisms that can multiply in the body, so they cannot infect an unborn baby in the womb. (Public Health England)
Find out more with these two resources:
Government Guidance
Royal College of Obstetricians & Gynaecologists
Vitamin D supplements
During the Autumn and Winter months, the Government has advised people who are “clinically extremely vulnerable” to take a supplement of vitamin D every day to support general health and in particular for bone and muscle health.
Many of us have been indoors more than usual this year and so might not have been making enough vitamin D from sunlight. You can find general advice on vitamin D here: https://www.nhs.uk/vitamin-d
If you have received a letter from the NHS Department of Health and Social Care (DHSC) you may be entitled to a free 4-month supply of daily supplements of vitamin D. If you have done so, and would like to opt-in to receive your free supply of vitamin D, you will need register your details between 30 November 2020 and 4 January 2021 at the following link: https://www.nhs.uk/get-vitamin-d
If you have not received a letter saying you’re at high risk from coronavirus and think you should have, or if you have any concerns please speak to your healthcare professional.
Initial Data (up to January 20th 2021) – Patient information on COVID-19 in haemoglobinopathy and rare inherited anaemia patients
 Since the start of the COVID-19 pandemic, some groups of patients have been classed as ‘clinically extremely vulnerable’ and advised to ‘shield’ in order to avoid becoming infected. Many patients and patient support groups would like know how frequent and how severe COVID-19 has been for people with inherited anaemias, including:
Since the start of the COVID-19 pandemic, some groups of patients have been classed as ‘clinically extremely vulnerable’ and advised to ‘shield’ in order to avoid becoming infected. Many patients and patient support groups would like know how frequent and how severe COVID-19 has been for people with inherited anaemias, including:
- Sickle cell disease
- Thalassaemia (transfusion dependent and non-transfusion dependent)
- Diamond Blackfan anaemia
- Congenital dyserythropoietic anaemia
- Congenital sideroblastic anaemia
- Pyruvate kinase deficiency (with and without a spleen)
- Hereditary Spherocytosis (with and without a spleen)
- Other types of rare inherited anaemia
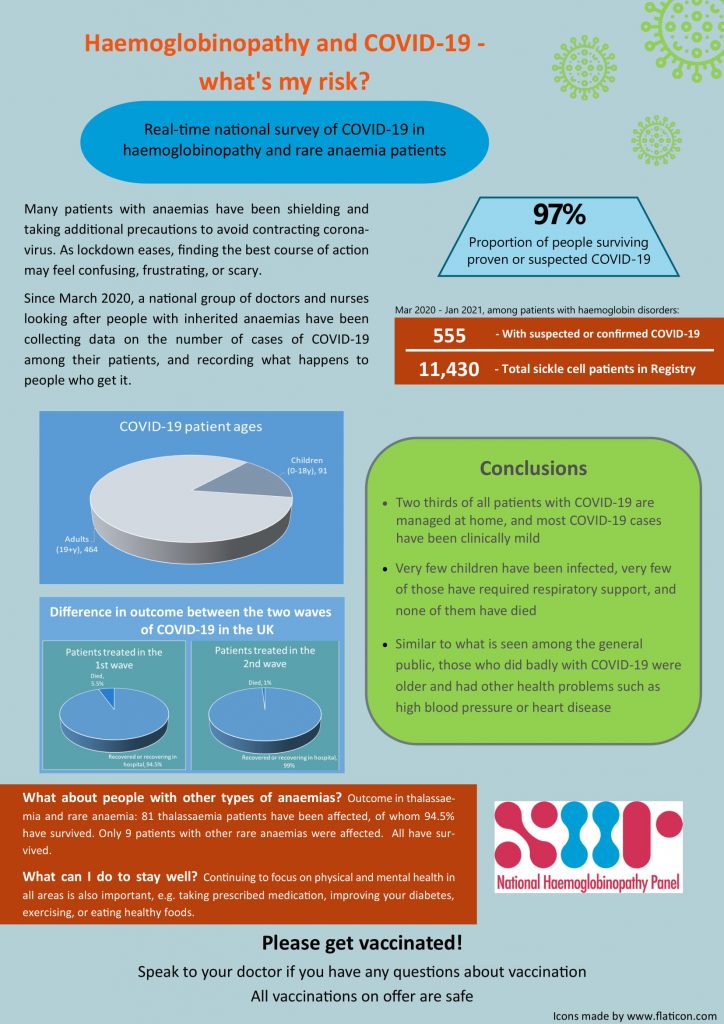
Since March 2020, a national group of doctors and nurses looking after people with inherited anaemias (called the National Heamoglobinopathy Panel) have been meeting via videoconference once a week to discuss how COVID-19 has affected their patients. This discussion is entirely confidential, with no patient-identifiable details discussed at all. The group reviews guidance issued by NHS England and advises NHS England and patient support groups about specific COVID-19 risks. Hospitals across the England have sent in anonymised data to the group regarding the number of cases of COVID-19 and what happens to people who get it.
How many people with inherited anaemias have had Covid-19?
As of January 20th, 555 people had been reported with proven or suspected COVID-19. Of these, 464 were adults and 91 children. Most had sickle cell disease, and some thalassemia and rare inherited anaemia patients were also affected, and the severity in all patient groups was similar.
How many people were admitted to hospital?
During the second wave, about 6 out of every 10 patients were admitted to hospital, and the rest (4 out of every 10) managed at home. More women than men were admitted to hospital (3 women for every 2 men). Of those admitted to hospital fewer than 5 in every 100 needed intensive care.
What are the risks for children?
Of the children suspected or proven to have COVID-19, very few suffered serious complications or required intensive care. Children with sickle cell disease, thalassaemia and rare anaemias who do not have other risk factors, do not seem to be at increased risk of having severe disease.
What was the outcome for people admitted to hospital?
The picture is not yet complete, because some people are still being treated for COVID-19. The information is updated regularly. For the moment we can say that:
- the available results show that for every 100 patients infected, 97 (97%) have recovered or are still in hospital, and 3 (4%) have died
- the people who died were more likely to have other medical problems such as heart disease, cancer, kidney disease, diabetes and high blood pressure
- it is too early to say whether patients with inherited anaemias do any worse than the general population
- adults with sickle cell disease should still be considered ‘clinically extremely vulnerable’ and follow government guidance about shielding
- in the case of adults with thalassaemia and rare anaemias, the advice on shielding should be assessed for each person by their doctor
- it is important to note that there have been many people with inherited anaemias who have had few or no symptoms with their COVID-19 infection, and who have fully recovered
What do I do if I think that I or my child may have Covid-19?
Please do not stay at home without telling anyone– it is important to contact your medical team and discuss whether or not you should be assessed in hospital.
Isn’t coming to hospital dangerous?
There are many people who have been extremely concerned about presenting to hospital, some have delayed at times when they have been very unwell. If someone with these important health conditions is unwell, please seek advice from your specialist team. Hospitals have been re-organised to protect people who come in with non-COVID admissions.
What can I do to stay well?
We recommend that continuing to focus on physical and mental health in all areas is also important eg taking prescribed medication, improving your diabetes, exercising, or eating healthy foods.
If you have any concerns about you or your child’s individual risk please discuss it with your specialist team.
Finally, please get vaccinated (whichever vaccine you are offered) when this is offered to you by your GP. This will greatly decrease your chance of getting infected or suffering serious consequences of COVID. Speak to your doctor if you have any concerns about vaccination.
Continue reading for the official guidance and advice
Keeping Healthy
Given the very unusual circumstances that shielding creates, it is important to be aware of ways to keep oneself as fit and healthy as possible. This includes eating a varied diet which should include plenty of fresh fruit and vegetable. Foods that contain Vitamin D such as oily fish and eggs are important as Vitamin D deficiency is very common not only in the general population but also in sickle cell disorder and may exacerbate bone pain. Sunlight on bare skin is a good way to increase Vitamin D intake so every opportunity should be taken to benefit from the sun, if only at an open window or on a balcony, if sitting in a garden is not feasible.
Taking regular moderate exercise is not only good for physical health but also improves general mood and helps overall mental health. Very rigorous exercising is not recommended in sickle cell disorder and if the weather is hot care should be taken to drink plenty.
If you are anxious about your health whilst shielding or want more advice you can contact your specialist health care team . If you become unwell you should contact your GP and in an emergency phone 999.
To get support for mental health visit: https://www.nhs.uk/oneyou/every-mind-matters/
Hospital and GP Appointments
Where possible, try and access medical assistance remotely. Hospital care teams are offering most patients telephone or video consultations during the COVID-19 outbreak.
If you have a scheduled hospital or other medical appointment and have not been contacted by your GP or specialist about this, call them before attending to confirm that the appointment has not been canceled or postponed. Talk to them about how best to ensure you can continue to receive the care you need.
Children and Young People
Specialists in paediatric medicine have reviewed the latest evidence on the level of risk posed to children and young people from COVID-19.
The latest evidence indicates that the risk of serious illness for most children and young people is low. In the future, we expect fewer children and young people will be included on the shielded patient list.
If a child or young person is removed from the shielded patient list, they will no longer be advised to shield in the future if coronavirus transmission increases.
To decide on whether a child or young person should be removed from the shielded patient list, you should talk to your paediatric specialist or GP.
Post-Covid Inflammatory Syndrome
Specialists in Italy and England have described an increase in cases of an paediatric inflammatory multisystem syndrome (similar to Kawasaki disease) following the beginning of the pandemic with COVID-19*. This is a very rare syndrome characterised by a high temperature, rash and swollen glands. The treatment includes the use of high dose steroids and the outcome is usually good.
However, this treatment could be detrimental in children who have sickle cell disorder. It is important therefore that a distinction is made between a sickle cell episode and this very rare disease. There can be confusion as symptoms overlap. It is important that you talk to your specialist paediatrician or haematologist if you are concerned about new symptoms occurring weeks after a Covid infection to ensure the right diagnosis is reached.
*BMJ 2020; 369 doi: https://doi.org/10.1136/bmj.m1990 (Published 15 May 2020)
Sickle Cell Trait
If you have sickle cell trait please follow the guidance given to the general public. This doesn’t make you more vulnerable to coronavirus infection but do check the full clinically vulnerable groups list in case you fall into another category such as if you have had your spleen removed, are pregnant or aged over 70). The full clinically vulnerable groups list can be found here.
General Advice about Feeling Unwell
If you are mildly unwell with a cough or fever below 37.8 oC you should manage your illness at home and not go to your GP or A&E. If you are worried about your symptoms you should call your hospital care team for advice.
If you suspected you have any symptoms of COVID-19 (high temperature and/or new and continuous cough) please contact your centre (even if you have called 111) of care to ensure that you receive the appropriate specialist advice on the need for further assessment.
Due to the impact other infections can have on people living with sickle cell (including pneumonia and acute chest syndrome) anyone with a sickle cell disorder who has a worsening cough, difficulty in breathing or fever above 38 oC should urgently contact their centre of care or in an emergency 999. Mention you are worried about coronavirus but also that you have sickle cell disorder. They will then instruct you further.
Sickle Cell Pain (Crisis)
If you are experiencing severe sickle cell pain (crisis) then go to hospital as normal. However, if you also have a cold, a high temperature or new and continuous cough contact your centre of care (or 999 in an emergency) first.
Taking medicines during the COVID-19 outbreak
If you are taking hydroxycarbamide or iron chelators (drugs to remove excess iron) it is important these are continued. Your centre of care will make arrangements to monitor this treatment through the hospital or your GP. There is no evidence these drugs affect the risk of COVID-19 one way or the other. However there is some concern that anti-inflammation pain killers like ibuprofen might make coronavirus infection worse. During the COVID-19 outbreak it is recommended that you take paracetamol (unless you have an allergy to it) which is safe instead.
To avoid the catching or spreading of germs:
- cover your mouth and nose with a tissue or your sleeve (not your hands) when you cough or sneeze
- put used tissues in the bin immediately
- wash your hands with soap and water often – use hand sanitiser gel if soap and water are not available
- try to avoid close contact with people who are unwell
Don’t:
- do not touch your eyes, nose or mouth if your hands are not clean
The NHS have a specific service for people who think they might have coronavirus. You can find out more about it here: https://111.nhs.uk/covid-19
Do not go to a GP surgery, pharmacy or hospital. Call 111 if you need to speak to someone or use the online service.
Responding to Covid-19: Reasons for Hope
Sickle Cell Society Chief Executive, John James OBE, writes for the King’s Fund’s Leading through Covid-19 series to reflects on the challenges the organisation has faced and shares what he has learnt and what gives him hope for the future. Click here to read the full article.
Official guidance and information can be found here:
NHS – https://www.nhs.uk/conditions/coronavirus-covid-19/
GOV.UK – https://www.gov.uk/government/topical-events/coronavirus-covid-19-uk-government-response
Key Links
111 Online Service: https://111.nhs.uk/covid-19
Employment: https://www.gov.uk/government/publications/guidance-to-employers-and-businesses-about-covid-19
Extremely Vulnerable Group: https://www.gov.uk/coronavirus-extremely-vulnerable
Government Response – https://www.gov.uk/government/topical-events/coronavirus-covid-19-uk-government-response
Isolation Advice: https://111.nhs.uk/isolation-note
Local Support: http://www.gov.uk/coronavirus-local-help
Mental Health Support: https://www.nhs.uk/oneyou/every-mind-matters/
NHS Guidance – https://www.nhs.uk/conditions/coronavirus-covid-19/
Support for Buisnesses: https://www.gov.uk/government/publications/guidance-to-employers-and-businesses-about-covid-19/covid-19-support-for-businesses
Universal Credit and Coronavirus: https://www.understandinguniversalcredit.gov.uk/employment-and-benefits-support/